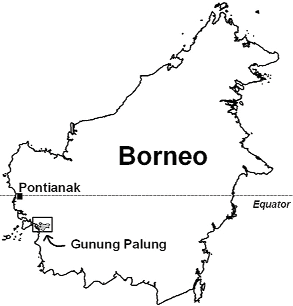
In November 2007 I (David Werner) had the opportunity to visit Health in Harmony, an innovative new program in a remote area of West Kalimantan, on the Indonesian portion of the island of Borneo. This pioneering program is crucially relevant to our imperiled times because it strives to address, in an integrated participatory way: 1) the pressing health needs of the local villagers and 2) the environmental protection of endangered tropical forests. In a holistic manner, it combines community-based health care with the overarching issues of deforestation, global warming, and the conservation of the intricate balance of life.
In the words of the program founder, Kinari Webb, “Health in Harmony is inspired by the recognition that global health for all depends on linking human and environmental health at the local level.”
Health in Harmony: a Program in Borneo that Links Community and Environmental Health
The Making of the Dream: Curious Parallels
When Kinari Webb, the young North American co-founder of the Health In Harmony program in Borneo, first visited the rainforests of Kalimantan as a college student 15 years ago, she carried in her backpack a copy of my village health care handbook Where There Is No Doctor. Deep in the Borneo jungles she had used the handbook to treat both her own ailments and those of local villagers. In the process she began to form a far-reaching dream. Her plan was to study medicine and some day return to Indonesia to launch a back woods health initiative, where people would work together to safeguard both their own well-being and that of the natural environment: Health for All in an all-inclusive sense!
There are curious parallels with regard to how Proyecto Piaxtla in Mexico and Health in Harmony in Indonesia got started. Both Kinari and I had backgrounds in the biological sciences. It was our love of wilderness that lured us to corners of the earth rich with biodiversity and exotic beauty. Back in 1964, when I was in my late 20s, I visited the remote reaches of Mexico to study the birds and plants of the Sierra Madre Occidental. Four decades later, in 1993-94, young Kinari went to the Gunung Palung National Park in West Kalimantan to study the endangered orangutans in the tropical rainforests there. Initially, on our respective expeditions, neither Kinari nor I had any idea of getting involved in community health care. As had happened to me in the mountains of Mexico, so Kinari in the wilds of Borneo was deeply moved by the warmth and friendliness of the local people—and also by the enormity of their health needs.
Oneness Through Diversity
From the time she was a young girl in New Mexico, Kinari had always felt a love of wildlife and a strong empathy for creatures that were mistreated or endangered. On finishing high school, she majored in human biology at Reed College, an idealistic forward-looking university in Oregon. Inspired by the efforts of Jane Goodall, she developed a strong interest in the primates, and a desire to protect them. It was this interest that motivated her to take a year off between her junior and senior years to study the waning population of orangutans in the tropical rainforests of Gunung Palung National Park in Indonesia.
Orangutans are one of the primates closest to human beings in terms of their intelli- gence, behavior, and DNA. The indigenous people of Borneo recognized the resemblance of these intriguing apes to people, which is why they named them orangutan—or “persons of the forest.” During her research Kinari studied the many ecological factors that were—and still are — threatening the orangutans with extinction.
In her study of the orangutans Kinari became acutely aware of the important role these great apes play in the ecology of the forest. This led to an appreciation of the interconnectedness of living things, large and small. Indeed, the more we learn about the planet’s intricate web of life, the more we learn that an ecosystem is like a living organism, in which the wide diversity of species, massive to minuscule, all play their part. The loss of any entity diminishes the whole.
Most traditional tribal people have instinctively realized this. “Civilization,” however, has built walls separating us from the world of nature, and from each other. Because of this fragmentation, it is easy for us to forget that we are an integral part of a single living whole. The loss of awareness of that oneness— of the interconnectedness for the common good of all that lives and breathes—is fast driving our species, and many others with us, toward the brink of extinction.
Kinari became acutely aware of this “oneness through diversity” during the year she spent in the jungles of Kalimantan.
A Formative Moment
In one of my discussions with Kinari, I asked her if there was some particular incident that had catalyzed her dream to study medicine and return to set up a village health program in Borneo. She told of an event that happened deep in Gunung Palung rainforest. Her account of it went something like this:
One afternoon a man came into the forest clearing with a big cut on the palm of his hand. He was scared to death, and I wondered why. Although the wound was deep no tendons had been cut. Then I realized that for the local people living deep in the jungle, with no medical services within miles, and with no money to get to a far away clinic or pay for medicines, even minor injuries often got infected and were life-threatening.
In all honesty, I shared his fear. I’d never treated a big open wound like that. So I pulled out my copy of Where There Is No Doctor and looked up “Treatment of Wounds.” Following the guidelines, I cleaned the wound and closed it carefully with improvised butterfly bandages I made of adhesive tape. To my great relief the wound healed fine! Slowly it dawned on me that medical care wasn’t some magic power reserved for god-like practitioners.
That was when I first thought of studying medicine and returning to serve the people.
Liaison of the Love for Health and Environment
Another happenstance strongly influenced Kinari’s determination to return to the rain Forests of Kalimantan. While camping at the remote research station in Gunung Palung, she met a botanist/ecologist named Campbell (Cam) Webb. The two shared many of the same interests, and together they began to weave a dream of someday returning to Indonesia to play a role in protecting the health of both the endangered rainforests and the people living in them.
On her return to the US, Kinari completed her last year at Reed College. After graduation she married Cam and applied to Yale Medical School, where she studied hard and was at the top of her class. During vacations, whenever they could, she and Cam returned to the jungles of Indonesia. Kinari graduated from medical school with distinction. From there she went to Contra Costa Regional Medical Center in Martinez, California, which has one of the best Family Practice residencies in the country.
### The Tsunami
On December 25, 2004, when Kinari was in her last year of residency, a horrendous tsunami occurred in the Indian Ocean, setting off a tidal wave that killed 267,000 people, more than 200,000 of them Indonesian. When she asked for a leave of absence, they not only approved, but also raised money to cover her expenses, as her residency’s contribution to the relief effort. Kinari spent 6 weeks at Aceh, Sumatra, in the beach community hardest hit by the tsunami. Ninety percent of the people there were killed. Bodies were still strewn everywhere, as there were too few able bodied people left to remove them. Thousands of injured and hungry people were hunting through the rubble for loved ones, or just trying to survive. It was the most distressing experience in the young doctor’s life. Kinari worked around the clock doing what she could to help the injured and suffering.
While in Aceh, Kinari had a chance to observe international relief agencies in action— scores of agencies and organizations, government, non-government, and international. She saw that much of their work was ineffective—largely because they seldom listened to the people to find out what they most needed and wanted. It was in Aceh that Kinari decided, if she ever set up a clinic, she would seek the involvement of the people being helped.
After her harrowing experience in Aceh, Kinari returned to her Family Practice training in California and completed her residency.
A Productive Visit
Kinari picks my brain In the summer of 2005, during an excursion across the US, Kinari visited me at my summer hideaway in New Hampshire’s White Mountains. She explained to me that my writing had been instrumental in her decision to set up a community health program in Indonesia’s endangered rainforests. She grilled me about the planning, community involvement, training of workers, management, and the successes and failures of the Mexican program. Above all, she questioned me about how the village health program in Mexico was financed. In one of my newsletters, from back in the late 1970s, she had read about the unique “Payment with Work” scheme we had introduced, in which people could pay for health care either with money or with work. She and her husband had decided to use a similar scheme in the health program they were preparing to launch in Indonesia. Their intention was that the poor people in the villages surrounding the endangered rainforest could pay for their health care through work that would help protect the forest.
After considering a number of options, Kinari and Cam settled on the place where they had first begun their biological research work, as the site of the clinic. This was on the coastal side of the Gunung Palung National Park in Kalimantan. Fund-raising was a major challenge. Fortuitously, to help cover their expenses, Campbell Webb was offered a job by Harvard University, researching the trees and biodiversity of Indonesian rainforests.
|
|
|
Invitation to Visit Kalimantan
In spring of 2007 I received a letter from Kinari Webb informing me that the Heath in Harmony program had at last become a reality, and was already showing great promise. She invited me to visit as a consultant, primarily on the payment-with work approach, which they’d already started—but which was still not working as well as they had hoped. I jumped at the chance to visit this innovative program in the Indonesian rainforest. I was especially intrigued by the chance to observe first hand a project that combined community health with environmental protection.
Arrival
The village of Sukadana, where the Health in Harmony program has its base, is—to say the least—remote. To get there from California took the better part of five days on a number of flights and a long drive into the mango swamps. My journey was all the more challenging because in addition to my personal baggage I transported a large, donated, portable dental chair that had landed on my doorstep the evening before I left. But when I turned the chair over to Hotlin, the young Indonesian dentist who helps manage the Health in Harmony program, her ecstatic delight made all the lugging and sweat worth it.
I found that although the program had only been running for 5 months, the results were already impressive. A team of 14 health workers had converted a large rented house artfully converted into a makeshift health center. This is located a mile outside the main village of Sukadana, near the beach on the eastern edge of the Gunung Palung National Park. The health center is called the ASRI Klinik. The word asri means “beautifully and harmoniously balanced.” But ASRI is also an acronym for Alam Sehat Lestari, which translates as Nature and Health Everlasting—the Indonesian paraphrase of Health in Harmony with Nature.
Warmth and Openness of the People
I was delighted by the friendliness and uninhibited good will of the people uninhibited good will of the people I encountered in West Kalimantan. At the Klinik or along the roads—though I was a complete stranger to them—people would smile and greet me warmly, even the young children. Young men passing by on their motorbikes, which outnumber cars 100 to 1, would slow down and offer me a ride.
As I came to know the people better, I was impressed by the easy-going relationship between men and women, old people and young people, and especially between adults and children. Although in the villages near the ASRI Klinik the majority of the people are Moslem, there was no indication that harsh restrictions were imposed on women’s social liberties or dress. In the village meetings women outnumbered men, and often took the lead in the discussions. Also, mothers were completely at ease with breastfeeding their babies in public. One staff member I talked to at the ASRI Klinik referred to the type of Muslim religion practiced in this part of Indonesia as “peaceful Islam.”
This non-repressive pattern toward women was complemented by the relative lack of aggressive posturing or machismo on the part of the men. There is little question that in the villages of West Kalimantan there is far less violence than that which commonly occurs in Mexico and much of Latin America. Part of this striking difference can no doubt be explained by the very limited use of alcohol in the Muslim communities, compared to Christian ones.
But there may be other reasons as well. A number of comparative studies have shown that children who are brought up in a child-friendly, non-repressive way, where there is a lot of touch, bodily acceptance, and personal warmth, tend to grow up to be gentler, more humane, and less aggressive adults. Likewise, societies that have more permissive, child-friendly, curiosity-accepting customs of raising children, tend to be more peaceful and harmonious, and less belligerent.
|
|
|

[CAPTION][CAPTION]
In West Kalimantan, young children grow up in a very child-friendly, non-restrictive environment. From an early age, they intermingle and seem comfortable with adults, even strangers. Although the children showed a lot of curiosity and amusement with what was new and different, they were surprisingly considerate and non-disruptive. Never did I see any parent scolding a child or threatening disciplinary action. On the contrary, I observed a great deal of physical closeness, hugging and touching, between children and grown ups, and among the children themselves.
Yet for all this easygoing, convivial warmth at the personal level, the larger society has its stark contradictions. The power structure appears to be very hierarchical and rigidly authoritarian. Indonesia also has a recent history of tyrannical rule and violent oppression of dissent.
Beginning with Curative Care
Kinari decided to start her program with a focus on curative care. Her rationale was that by beginning with a focus on treatment—which is what most people feel they most urgently need—it is easier to get the whole community eagerly involved in the new program. Then, once people are engaged and participating, the program’s focus can be extended to preventive measures, organized collective action, and environmental protection. Already in just five months, the ASRI Klinik had treated over 1200 villagers.
Epidemiology
Unusual Patterns of Disease
As an American physician, Kinari is still trying to gain an understanding of the epidemiology, or “pattern of sickness and health” in this remote corner of Kalimantan. Similar to many poor countries in recent years, infectious disease is still common—including some diseases as ancient as leprosy.
In addition to the infections and “diseases of poverty,” in the last few years there has been a dramatic increase in the chronic diseases that have become the big killers in richer countries, namely high blood pressure, heart disease, stroke, diabetes, and cancer. In richer countries—and increasingly in many poorer countries as well—these chronicills are typically associated with obesity. In Kalimantan, however, this is not the case. Surprisingly, most of the people who come to the ASRI Klinik with high blood pressure, heart disease, and diabetes are not overweight, but thin. Furthermore, the onset of high blood pressure, stroke, and type 2 diabetes often presents in relatively young persons, not uncommonly in middle age.
Kinari and the ASRI team have tried to explain these unusual findings. They strongly suspect poor diet and high sugar consumption are contributing factors. The cost of the main staple, rice, has risen so much that poor people get more and more of their calories from sugar, often in the form of junk food and heavily sweetened drinks. The high consumption of such junk foods is evident from all the discarded plastic containers and wrappers that litter the grounds in front of the Klinik every morning. Not surprising, extensive tooth decay, starting in young children, is a ubiquitous problem.
Diabetes
Diabetes in West Kalimantan is a big and growing problem, unrelated to obesity. Often it is diagnosed late, only after serious complications have begun. One example is Pak Tahir, a middle-aged man who arrived at the Klinik with a huge badly infected diabetic ulcer on the back of his hand. He had been turned away from the government clinic, being told the ulcer was untreatable and the hand had to amputated. For such an operation he would have had to go to a distant city, which he couldn’t afford. On his arrival at the ASRI Klinik, his hand was terribly swollen; the gaping ulcer left the tendons and nerves in his hand exposed.
Kinari, too, was afraid the hand might have to be amputated – but decided to first try to save it. They put the man on high doses of antibiotics, brought his blood sugar level under control, and patiently began the long slow process of debriding the putrid flesh. When I first visited the Klinik a week after treatment began, already the infection was largely under control and a bit of granulation had begun around the borders of the ulcer. But the hand was still badly swollen and looked awful.
I suggested using honey to treat the ulcer. At PROJIMO, our backwoods rehabilitation program in Mexico, we have had excellent results applying honey to pressure sores, intractable skin ulcers, and severe burns. Studies now exist that substantiate the effectiveness of this treatment. Since traditional healers in Kalimantan have long used honey for treatment of chronic wounds, the man was eager to try it. Within a few days the enormous ulcer was healing much faster. Everyone was duly impressed. “I think we’re actually going to save his hand!” said Kinari. “At first I didn’t think there was much hope.”
Tuberculosis
One of the major health problems in the impoverished villages served by ASRI Klinik is tuberculosis. Scores of persons with advanced TB have come to the Klinik for treatment. Kinari estimates that up to 30% of the local population has active tuberculosis, and that virtually the entire population has been exposed.
Although the government tried to minimize the severity of the problem, many of the people who come to the Klinik with active TB say they have, in fact, already been treated. Unfortunately, in most cases their treatment was incomplete. Too often, when they began to feel better, they stopped taking their medicines. With so much interruption of treatment, the probability that resistant strains of TB will emerge is high.
To combat the high incidence of TB and the low completion rate of treatment, the ASRI team is determined to start a Direct Observation Therapy (DOTS) program. They are in the process of recruiting responsible members of the community to oversee the treatment of all persons receiving TB medicines. This entails visiting their homes 3 times a week for 6 months, to directly watch them taking the necessary combination of pills. In selecting candidates to work in this program Kanari emphasizes that they need to have a warm, supportive attitude and relate to their pill-taking clients as equals.
I asked whether the soaring incidence of TB might be related to an increase in HIV/AIDS. No one could say for sure, but it appears that the incidence of HIV is quite low. If so, this might be related to their religious beliefs, which lead Moslems to have fewer extramarital sexual contacts than those in the other dominant belief systems.
Cancer
Undoubtedly, in West Kalimantan, smoking contributes to the high incidence of cancer, which often begins at a relatively early age. But smoking does not account for the unusually high incidence of some other cancers, such as naso-pharyngeal carcinoma. The ASRI team suspects that the high cancer rates may in part be caused by the wide use of dangerous brands of pesticides and herbicides. Toxic and carcinogenic chemicals banned in most countries are still widely used here. Because governmental regulations are weak, and poorly enforced due to under the-table payoffs and corruption, transnational agrochemical companies routinely dump their noxious products in Indonesia.
A further likely cause of elevated cancer rates comes from illegal use of formaldehyde (formalin) as a preservative for fish and tofu. Because it is cheaper than ice, thousands of poor fishermen in their dinghies use formaldehyde to extend the time their fish will last before they spoil in the sweltering heat.
For this reason, in Indonesia a unique public health message is circulated in fish markets: “Only buy fish if flies are buzzing around it.” Apparently flies have a better nose for health hazards than people. They won’t go near fish preserved with formaldehyde. For all its bureaucratic policing, Indonesia is amazingly weak when it comes to enforcing the laws to protect the health of people and environment.
Ecological Challenges
The Destruction of the Rainforest and Peat Swamps
Most of the villages surrounding the National Park are situated in lowland man grove swamps, which in some places extend inland in for miles. Most houses are perched on wooden stilts over the brackish water that rises beneath them with the tides. In such a salty, soggy environment, family gardens are out of the question. It is little wonder so many people are unaccustomed to eating vegetables!
Work options for dwellers in the salt marsh are few. Tens of thousands of impoverished people manage to subsist through illegal timbering. A huge portion of the Gunung Palung National Park has already been timbered beyond recovery. On the more accessible slopes of the Park’s westward margin, vast areas have been clear-cut (timbered completely) and a monoculture of a very hardy invasive species of grass called alang-alang has taken over. Once this imported grass takes hold, no other plants can successfully grow there. Every dry season the grass catches fire and burns up the tree seedlings that are trying to repopulate the devastated land. The next rainy season the grass grows back again and the pervasive monoculture continues.
Deeper into the rainforest clear-cutting is less common. And fortunately, the forest service now has more stringent controls. Nevertheless, huge numbers of commercially valuable trees continue to be felled by an army of impoverished villagers from the lowlands. Thousands of timber poachers scramble through the forest, cutting down prized trees, such as the Borneo ironwood. They drag the wood out of the forest by any means they can contrive, including cutting it up into planks or beams that are carried out on their backs.
Most of the timber poachers are too poor to purchase the chainsaws used to cut the trees. Instead, they work for “log bosses,” who rent them the saws. For their illegal, exhausting and dangerous work in the forest, the tree poachers are paid under US$2.00 a day. Meanwhile the log bosses make a fortune on resale of the wood.
Fires
Peat moss—which has built up slowly over tens of thousands of years—is in some places over 20 meters (65 feet) thick, and covers thousands of square miles. Dry peat becomes a tinderbox. When the peat catches fire—or is intentionally set on fire for “slash and burn” land clearing—the fires spread, both on the surface and underground, where they are very hard to control.
The draining and burning of the lowland peat forests began decades ago with the introduction of rubber tree farms. During the last decade this decimation has increased dramatically with the proliferation of palm oil plantations. As these vast areas of ancient peat bogs are consumed by logging and fire they pour huge amounts of carbon dioxide back into the air, contributing massively to the greenhouse effect and global warming.
This unbridled environmental demise is no trivial matter. Indonesia is listed in the Guinness Book of World Records as having “the world’s highest rate of deforestation.” The combination of massive deforestation and burning of huge peat bogs puts Indonesia as the world’s third biggest contributor to global warming, after the USA and China! It has been calculated that the destruction of peat swamps currently accounts for 10% of the carbon dioxide emissions contributing to global warming.
Biofuels as a Contributor to Global Warming
Palm oil is now produced mainly for use as a bio-fuel. While the monoculture plantations in Indonesia do provide a limited amount of employment, the pay is very low—sometimes as low as $0.50 a day. All the profits go to a few wealthy businessmen, and the end product feeds motor vehicles rather than people. Ecologists and students of climate change argue that decimating the rainforests and peat swamps to produce bio fuels is a great step backwards in terms of combating global warming.
Search for Solutions
There are no easy answers to the ecological dead end that has emerged in West Kalimantan and similar places in Indonesia. Indonesia is the world’s 4th most populated nation, after China, India, and the USA— although it ranks 22nd in terms of its economy. The island of Java alone has a population of 100 million people—a third that of the United States—in an area the size of the state of New Jersey. The capital city, Jakarta, now has over 20 million people, and keeps growing—as does massive job lessness and destitution. The government’s urgency to export its surplus of indigent people to the less populated isles is understandable—even if in the long run it is counter-productive.
For all their vast biodiversity, the islands to which many people were sent simply cannot support a large population of human beings. Unless the millions of families transplanted to these islands are given non-agricultural job alternatives, the hopes of controlling the rampant logging of the rainforests are remote. A few moneymaking alternatives have emerged. Unfortunately, two of the new big businesses in West Kalimantan—palm oil plantations and bird-nest soup factories—are owned and controlled by a few wealthy people and do more to concentrate wealth than to provide income for the many.
Carbon Credits as an Alternative Income
Unless the impoverished people living in the lands surrounding the rainforests find other, more eco-friendly ways to earn their livelihood than by illegal timbering, one of the world’s most important carbon stores will literally go up in smoke. The destruction of Indonesia’s rainforests is not just the problem for Indonesia’s people. Ultimately it affects the whole planet and the future of all life upon it. The extinction of one of our closest relatives, the orangutan, may well be a harbinger to our own extinction.
It is from this holistic perspective that the Health in Harmony initiative is trying to strengthen the link between human and environmental health, and to introduce a plan of action whereby people can safe guard their health care by working to protect the environment. To date, in exchange for health services, people help clean the clinic, do laundry, wash equipment, and work in the experimental organic garden.
Currently the work the villagers do to pay for medical care does not begin to cover the costs of the consultations, much less the medicines they receive. However the hopes for the Work for Payment plan in the future are far-reaching. The goal of the program is to link efforts to protect the endangered rainforest to a comprehensive health insurance plan at the community level. The approach involves contracting the communities adjacent to the National Park to watch over and protect adjacent areas of the National Park. In exchange for assuring no logging takes place, the whole community will receive health care at no additional cost. The hope is that the village as a whole will pressure those individuals who previously cut timber to stop doing so, in order to secure the continuity of health care for all.
The HIH plan also involves reforestation and preserving of biodiversity through planting seedlings of the native trees in deforested areas, especially the endangered species. The hope is that these rainforest conservation activities will be done with the help of local villagers, partly as payment for health services.
The big question is where is the funding for such initiatives to come from? The HIH team is looking at “carbon credits.” The emerging international market of carbon credits is an environmental strategy designed to combat global warming. In this program, big corporations and industries that add a lot of carbon dioxide to the atmosphere are required to take measures to assure that an equivalent amount of CO2 is removed from the atmosphere and sequestered. To achieve this, the companies can engage in—or pay for—tree planting, fire fighting, or conservation efforts that reduce emissions of carbon dioxide. Alternatively, they can buy “carbon credits” from groups engaged in such greenhouse gas reducing activities. Already the carbon credit industry is developing its own kind of stock exchange, complete with brokers. Health in Harmony hopes to initiate a reliable system of forest protection and replanting, and once this gets duly accredited, sell carbon credits through an international broker.
If this carbon credit venture proves viable, it could be expanded so that the villagers surrounding the National Park could generate as much or greater income from protecting the rainforests as they currently do from logging them—in addition to having a built in health insurance program.
The Health in Harmony team realizes that for such a plan to succeed, the local communities must have a clear understanding of the issues and be fully behind it. To raise an awareness of the issues involved, the Health in Harmony program is now in the process of visiting all the 37 main villages surrounding the Park. In these villages it holds meetings or “focus groups” to analyze needs, discuss possible solutions, and get the people’s ideas and suggestions.
Visiting the Communities: Learning and Teaching
Preparation
One of Health in Harmony’s guiding principles is to listen to and involve the community as it looks for ways to protect the health of people and to safeguard the environment.
To this end the ASRI team invited me to take part in “focus group” discussions in three neighboring villages. In preparation for these meetings the team discussed possible methods to get the villagers to participate fully and to speak out about their biggest health-related concerns. I suggested two techniques that might be useful: (1) a “community diagnosis,” and (2) the “chain of causes” technique. Before setting out on our visits to the neighboring communities we spent some time learning how to use these techniques.
Participatory Community Diagnosis
In the community diagnosis the people from the community collectively list and discuss their most important health-related problems. To include persons who can’t read and write, this method—described in Helping Health Workers Learn—uses pictures rather than written words. Small drawings representing the problems different people consider most important are created. To each of these pictures symbolic figures attached that identify which sicknesses or health-related problems are :
-
most common,
-
most dangerous,
-
contagious, and
-
chronic or long lasting.
These four characteristics are symbolized, respectively, by small cut outs of
-
faces,
-
skulls and crossbones,
-
a sick face with arrows pointing to two healthy ones, and
-
a long wiggly arrow.
All these drawings of common problems with their corresponding features are placed in rows on the floor (or on a flannel-board) and discussed. Then ribbons are stretched between different problems to show how some lead or contribute to others. Through this activity the community members see and discuss the interconnectedness of their different problems. Invariably social problems such as poverty, low wages, and the high cost of medical care form hubs from which ribbons radiate out to many of the different illnesses and afflictions. Finally the villagers discuss what they can do, working together, to try to cope with some of the problems, and begin to confront the underlyin causes: Physical, Biological, Cultural, Economic, Political, and Environmental.
Exposing the ‘Chain of Causes’ Through the ‘But Why?’ Game
The second technique we decided to use in the village meetings focused on identifying the chain of causes behind the various health problems of the community. For this we planned to use story telling followed by the analytic “But why?” game. To demonstrate this participatory method to the staff of Health in Harmony, I used a modified version of the “Story of Luis” from our handbook Helping Health Workers Learn. This is a true story that relates how a long sequence of causes leads to the death, from tetanus, of a boy named Luis.
After listening to the story, the participants play the “But why?” game to reconstruct the series of events leading to undesirable outcome—in this case, Luis’s death:
“But why did Luis get tetanus?”
“Because he stepped on a thorn?”
“But why did he step on a thorn?”
“Because he didn’t have sandals.”
“But why didn’t he have sandals?”
“Because his father was too poor to buy new ones when they broke”
“But why was his father so poor?
“Because the topsoil on his riverside corn plot washed away in a big flood?
“But way does the river flood more than it used to?
“Because there is so much timbering in the mountains.”
“But why …?”
Etc. …
Following the “But why?” game, everyone pitches in to build a Chain of Causes, using a series of cardboard links, which lead from a figure of the boy with tetanus to an image of the grave. The links are marked with words and drawings to represent different categories of causes: physical (things), biological (worms and germs, etc.), cultural (beliefs and customs), economic (money) and political (who has power over whom). To these five categories of causes we now add the increasingly important group of causes, namely environmental. After building the chain, the group discusses which links could perhaps be broken—by individual persons or families, or by a community working together—in order to prevent other children also from dying of tetanus.
After practicing the “But why?” and Chain of Causes methodology, the Health and Harmony staff re-adapted the “Story of Luis” to fit the situation in west Kalimantan. They decided to also use “death from tetanus” as in the original Luis story, since tetanus still kills people in west Kalimantan because so few children and pregnant women get vaccinated (although the Constitution calls for universal coverage).
In revising the story, the staff wanted to give emphasis to the environmental causes of poor health, and help the villages discover how the destruction of the rain forests can contribute to poverty, sickness and death. So in their story, as a link in the Chain of Causes, they included the increasingly common crop damage caused by plagues of grasshoppers. In recent years, as the logging and wildfires have reduced forestland and replaced it with vast areas of monoculture alang-alang grass, huge clouds of grasshoppers have begun to swarm into the rice fields and fruit trees, stripping them bare. Building the grasshopper plague into the story and linking it to the logging of the rainforests makes it easier to piece together a more complete chain of causes. It becomes clear that crop loss, increased poverty, and lack of money for sandals and for medical care are all part of the chain of events that lead to the death of Eco. This more complete chain of causes made a convincing case for the need to take collective action to stop the illegal timbering.
The Village Meetings
Equipped with appropriate techniques for drawing out what people in local communities actually felt and thought, we set out to conduct preliminary “discussion forums” in three nearby villages. The meetings were well attended. At the third meeting more than 80 people were crowded into the small room we were using.
The use of the “But why?” technique in relation to the story of Eco was especially productive. When the group of villagers began to analyze which links of the chain they might break to prevent similar poverty-related deaths, they reflected on the high costs of medical care and how it increased their poverty. In turn, they saw how the shortage of money to pay for costly health services contributes to increased illness and death, since often they don’t get urgently needed care in time. People realized more clearly how the “Payment for Work” plan of the ASRI Klinik could help break the vicious cycle between health expenditures and poverty.
The “But why?” story with the Chain of Causes proved so effective in getting the villagers talking about their health needs and exploring solutions that the team decided to create another Chain of Causes story – this time about someone with tuberculosis to use with their DOTS workers.
Importance of Health Protecting Nutrition
Concern about good nutrition arose repeatedly in the discussion groups. Interestingly, although many families are very poor and many children are quite thin, severe life-threatening malnutrition in children appears to be less common than in many other poor countries. When I asked about this, people explained that in Moslem communities people believe in sharing with those who are in need. So extremes of hunger and malnutrition are uncommon, except in times of famine where everyone is affected. I have encountered a similar pattern in other Islamic countries, such as Egypt, where severe malnutrition is seldom seen.
The question of healthy versus unhealthy eating habits was of greater concern than under-nutrition. The ASRI medics pointed out that eating a great many sugar-loaded snacks put people at risk from such health problems as high blood pressure, strokes, heart attacks, diabetes and tooth decay. They stressed the importance of eating low-cost, health-protecting foods. Hotlin, the ASRI dentist, congratulated mothers for maintaining the traditional custom of breastfeeding their babies. But she pointed out the harm done by the “modern” practice of weaning their infants onto sweetened junk food.
Smoking
In the community diagnoses, at first the question of smoking did not come up. But when it did, the women, especially, spoke energetically about its negative effects on health. Some insisted that smoking was “contagious,” not because of second-hand inhalation, but because adults who smoke provide an insolubrious role model for children and adolescents. The women saw a link between smoking and poverty. The money spent on daily packs of cigarettes takes away from what the family has left for food, health care, and other basic needs.
Payment for Healthcare with Eco-Friendly Work
During the “community diagnosis” sessions several people pointed out that one of the most important factors contributing to poverty and poor health was, ironically, the high cost of medical services and medicines. One very thin woman with a little girl nestled in her arms explained that, before the ASRI program began, she and her neighbors often had to choose between spending what little money they had on medicine or food. But not any more! Now she can pay for the family’s healthcare with a few hours of work, without cutting into the household money needed for food.
Despite this enthusiastic feedback, the fact remained that most people who came to the Klinik—nearly 90%—still chose to pay with cash, not work. In the discussion it became clear that the amount being charged for services was so low that there was little incentive to use the work for services program. In this context, it appeared that to raise the fees would be in the interest of the program without denying anyone access to the services.
One important suggestion the villagers made regarding the “pay with work” plan was that they be able to work collectively, preferably on Sundays, to pay for their medical services. Working as a group, they said, would make it more enjoyable. This suggestion is being seriously considered.
One of the objectives of the payment-with-work option is to mobilize the community in environmental conservation work, such as tree planting and prevention of illegal timbering. While most felt this was a desirable goal, it was pointed out that for many people timber poaching was their only source of income. (See the Health in Harmony Newsletter, Dec 2007). The ASRI team’s plan for the future is to have virtually all of the work people do to pay for health services be directed toward protecting and revitalizing the rainforests. But this “eco-friendly” work initiative will take time to get fully underway. To date (Nov. 2007) the only environmental work project that has been started is the preparation of an experimental organic garden. Through this program the team is experimenting with ways to raise organic vegetables in a hot, humid tropical environment teeming with voracious insects and plant parasites.
### A Wealth of Good Suggestions
At first the people in the meetings were reticent to speak out. Often they said what they thought they were expected to say, rather than what they really thought or felt. This hesitancy to openly express their views is perhaps understandable in view of the fact that during the recent dictatorship in Indonesia over a million people were killed for speaking out and trying to stand up for their basic human rights. But once the villagers became engaged in the handson community diagnosis, they began to open up and speak from their hearts. Before long they were energetically discussing, arguing, laughing, and pouring out their bottled-up concerns. As they opened up, a wealth of good suggestions for coping with the many problems they face emerged.
Helping Ocu Walk
Before I arrived in Indonesia, Kinari had written me about a little boy who had great difficulty walking, asking if I would be willing to see and possibly help him. Since his family lives in a hut within walking distance of the Klinik, she took me to visit him the day I arrived. “Ocu has such a wonderful smile you’ll fall in love with him,” she said. And she was right. The program had not yet extended their services to include preventive and rehabilitation services to people with disabilities, but they were eager to learn.
Ocu (pronounced Achoo—something like a sneeze) was sitting on the steps outside his home when we arrived. He was eight years old, but small for his age. The boy apparently had meningitis or cerebral malaria when he was 4 years old, which had left his whole body stiff and spastic. He was proud to show how he had managed to learn to walk with the help of two poles. But spasticity and muscle imbalance in his lower limbs caused his ankles— especially the right one—to flop outwards, causing stumbling, loss of balance, and falls.
With a pair of high top shoes a visiting volunteer had bought for him, he could walk a little better, but still his ankles flopped over uncontrollably. We tried constructing him a make-shift pair of braces similar to the ones I use, but if anything they made it more difficult for him to walk.
Then we tried a very simple device: cardboard shoe inserts. Since his ankles tended to flop outwards when he took steps, we made a cardboard wedged-shaped shoe insert that was higher on the outer side. To our delight, when Ocu tried walking with the insert in his shoe, his right ankle no longer flopped over and he walked much better. But Ocu’s gait is still spastic, and will remain so. Walking with the two poles he tires easily. So Hotlin contacted a local carpenter, for whom I drew a sketch of simple wooden elbow crutches. Two days later the carpenter arrived with a pair of the most handsome crutches you could ever hope to see. Ocu was thrilled with his new crutches. Elbow crutches require lots of practice to get used to them. But Ocu is determined.
The next challenge will be to help the boy get an education. His physical limitations have made it difficult for him to get to school. Building a cart in which he could be hauled there, or the possibility of riding on the back of a bike were two options that were discussed. Whatever the answer, the Health in Harmony team and his family are committed to see that Ocu gets the opportunities for learning and inclusion he deserves.
Conclusion
Looking Ahead
In the 5 months since the ASRI Klinik was opened, an astounding amount has already been accomplished. Most importantly, the program has the enthusiastic support of the people, especially in the villages closest to the Klinik. It has the full cooperation of the National Park Service director. And with Kinari and Hotlin’s careful diplomacy, it is slowly winning the cooperation of the local health authorities.
Various new projects are under development. One idea for making the “Work for Payment of Healthcare” plan more inviting is to build a modest guesthouse next to the Klinik and near to the program’s experimental organic garden. That way, family members of sick persons who are interned at the clinic can stay in the guesthouse and work in the garden to work off the costs of health services.
Need for a More Comprehensive Health Plan
Kinari and the ASRI team agree on the need to extend the current health beyond its current focus on curative care, and to place more emphasis on preventive measures and community health promotion. During my visit we discussed possible ways to involve members of the community in various forms of health promotion. These included growth monitoring of young children, vaccination of children and pregnant mothers, health education of mothers and schoolchildren, and community campaigns aimed at reducing smoking and avoiding sugary junk foods and drinks.
One important area where the ASRI team has so far been largely uninvolved is in the inclusion and “rehabilitation” of disabled persons. Since this is a field in which I’ve been very involved, through PROJIMO in Mexico, and elsewhere, I was able to share ideas and suggestions with the ASRI team, as well as help with a number of persons with disabilities.
|
|
|
An Uphill Battle
If humanity is ever to overcome the enormous problems we naked apes have created through selfishness and disconnection, from one another and from the web of life, we must learn to live in harmony, with ourselves and with the ecosphere that surrounds us. We must affirm a oneness that in a paradoxical way supports our rich diversity. HIH is committed to this vision. It will be an uphill battle to realize their goal of unifying human and environmental health—but the team is off to a good start.
I hope that the strengths and vision of this pioneering program can serve as a catalystand springboard for a new, more sustainable, and more all embracing development Paradigm in the pursuit of Health for All.
To learn more about Health in Harmony, or to make a donation for their objective of “integrating essential medical care with environmental protection strategies for the threatened rainforests,” see http://www.healthinharmony.org/index.htm. Or write to Health in Harmony, 6114 LaSalle Ave. Suite 752, Oakland, CA 94611 USA.
NOTE: A longer, more extensive version of this report can be found on the HealthWrights website here.
End Matter
To help reduce costs and resource use, please subscribe to the Electronic Version of our Newsletter. We will notify you by email when you can download a complete copy of the newsletter. Write to newsletter@healthwrights.org.

| Board of Directors |
| Trude Bock |
| Roberto Fajardo |
| Barry Goldensohn |
| Bruce Hobson |
| Jim Hunter |
| Donald Laub |
| Eve Malo |
| Myra Polinger |
| Leopoldo Ribota |
| David Werner |
| Jason Weston |
| Efraín Zamora |
| International Advisory Board |
| Allison Akana — United States |
| Dwight Clark — Volunteers in Asia |
| David Sanders — South Africa |
| Mira Shiva — India |
| Michael Tan — Philippines |
| María Zúniga — Nicaragua |
| This Issue Was Created By: |
| David Werner — Writing and Photos |
| Jim Hunter — Editing |
| Jason Weston — Design and Layout |
| Trude Bock — Proofing |
Neither a lofty degree of intelligence nor imagination nor both together go to the making of a genius. Love, love, love, that is the soul of genius.
—Wolfgang Amadeus Mozart